Proximal humerus fractures are one of those injuries that orthopedic surgeons see again and again, especially in older adults with weaker bones. A simple trip and fall can cause a shoulder break in the elderly, while younger patients usually pick them up after high-energy trauma like road accidents. Treating these fractures isn’t straightforward. The surgeon not only has to bring the bone back into alignment but also preserve shoulder function, which is critical for daily use.
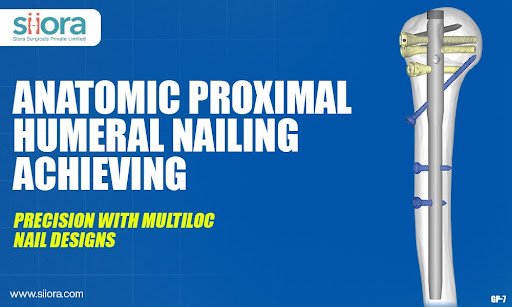
Over the last two decades, fixation strategies have shifted. While plates had their place, nails—specifically intramedullary nails—have emerged as a strong option. What makes them appealing is the smaller incision and the way they protect blood supply to the humeral head. That’s important for preventing long-term problems like avascular necrosis. But traditional nails had their weaknesses. Anyone who worked with them would remember the early issues—malalignment, screw loosening, and difficulty with tuberosity fixation. That’s where the newer anatomic Anatomic Proximal Humeral Nailing with multiloc features really step in.
Why the “anatomic” shape matters?
The humerus isn’t a straight rod of bone—it has curves and its own natural contour. Early nails didn’t respect this anatomy, and the result was a higher risk of irritation or even poor fracture reduction. Modern nails, however, are tailored differently. They’re made to fit the natural bow, meaning the implant sits where it should without fighting the bone. For patients, that often translates into less shoulder irritation and smoother recovery. For surgeons, it means fewer technical struggles in the OR.
Multiloc innovation explained in plain terms
When surgeons talk about multiloc technology, they’re usually referring to the concept of having several locking screw options near the top of the nail. Imagine trying to secure a tent pole in soft ground—you’d use stakes angled in different directions for better grip. The same principle applies here. Multiple screw paths, some divergent and some convergent, give stronger hold in osteoporotic bone.
Other useful design touches include dedicated holes for the tuberosities, options for improved angular stability, and solid distal locking. These features work together to stop the common complications we used to see—like screws backing out or the head collapsing in varus.
Day-to-day clinical benefits
What really matters is what the patient experiences afterward. Nails with multiloc options typically let patients start moving the shoulder sooner. Earlier mobilization reduces stiffness and helps them regain function faster. Elderly patients especially benefit because getting back to independent activity sooner reduces other health risks.
For the surgeon, stability is the biggest win. Reduction tends to hold better, even in multi-fragment fractures. And thanks to the minimally invasive technique, soft tissues remain undisturbed, vascularity is preserved, and healing improves overall.
Surgical pearls and pitfalls
Still, no implant alone guarantees success. Entry point precision, restoring tuberosity position, and careful selection of proximal screws matter in every case. Multiloc designs offer the options, but execution lies in the surgeon’s hands. The learning curve is manageable, but attention to detail prevents problems like joint penetration of screws or malalignment.
Looking ahead
Implants are evolving constantly. Some research now explores the combination of 3D planning with personalized implants for each patient. Others focus on new coatings that improve integration with osteoporotic bone. While future directions look exciting, the current generation of anatomic multiloc nails already provides a solid and dependable solution for many fracture scenarios.
Final thought
If you ask most surgeons today, they’ll agree that anatomic multiloc humeral nails represent a step forward from earlier options. They combine biology-friendly fixation with secure mechanical stability, which is exactly what’s needed in fragile bone conditions. In practice, that means less pain, quicker recovery, and a higher chance of patients regaining useful shoulder function. And ultimately, that’s the outcome both surgeon and patient are aiming for.
If you want to learn more about the advancements in the healthcare technology, including cutting-edge orthopedic implants, register for Arab Health.